5G technology is transforming healthcare by providing ultra-fast, low-latency, and high-capacity wireless connectivity. These features enable new models of care, enhance patient outcomes, and pave the way for innovations in smart hospitals, digital health platforms, and advanced medical devices.
Applications in Medical Networks
Telemedicine and Virtual Care
Real-time video consultations become more reliable, with higher-resolution streams and minimal latency, making remote diagnosis and care more effective.
Network slicing allows healthcare providers to prioritize mission-critical services, such as emergency care traffic or virtual ICUs, ensuring speed and reliability even during network congestion.
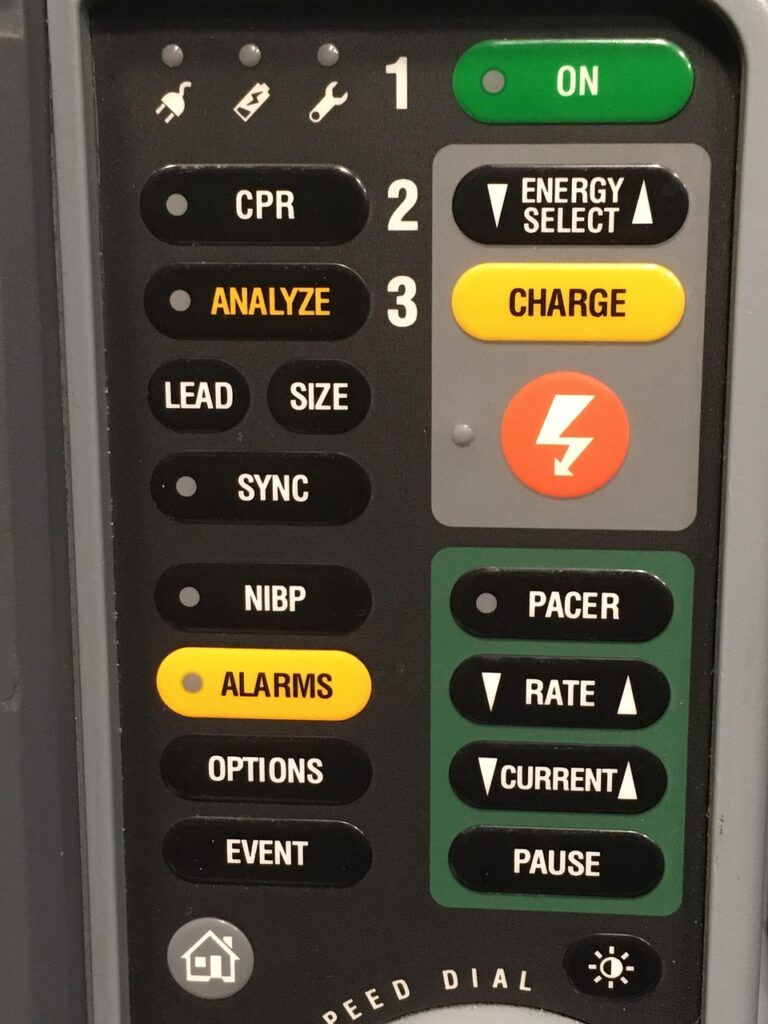
Remote Surgery
Robotic surgery benefits from 5G’s ultra-low latency; surgeons can remotely operate on patients with near-instantaneous responsiveness, allowing procedures to be performed across geographies.
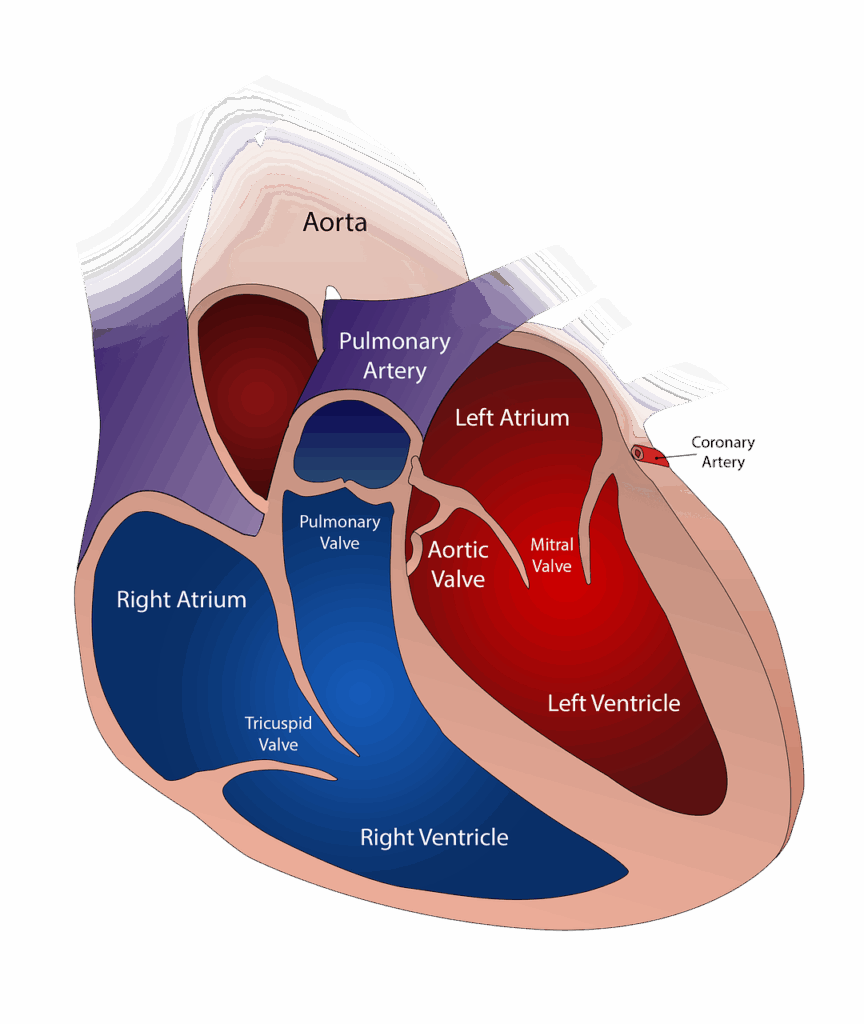
High-definition imaging transmission during operations is enabled by 5G’s broader bandwidth, supporting precise, guided interventions in real time.
Connected Ambulances and Mobile Care
5G-equipped ambulances transmit patient data, high-definition video, and vital signs to emergency departments ahead of arrival, improving preparedness and care for critical patients.
Digital Health Ecosystem Enhancements
Wearables and Continuous Health Monitoring
Wearable medical devices such as continuous glucose monitors, heart rate sensors, and oximeters leverage 5G for real-time, always-connected data streaming to healthcare providers.
Chronic disease management is improved, as clinicians can monitor conditions and receive alerts about anomalies, leading to timely interventions.
Artificial Intelligence & Data Analytics
5G enables large-scale, rapid transmission of medical data from devices to AI-powered analytics platforms, supporting predictive diagnostics, personalized care, and better treatment decisions.
Edge computing, supported by 5G, allows some AI functions to operate directly on devices, reducing both response times and data privacy concerns.
Implications for Medical Devices
| Application Area | Impact of 5G Technology |
| Remote patient monitoring | Real-time, high-fidelity data for chronic/acute conditions, enabling proactive care |
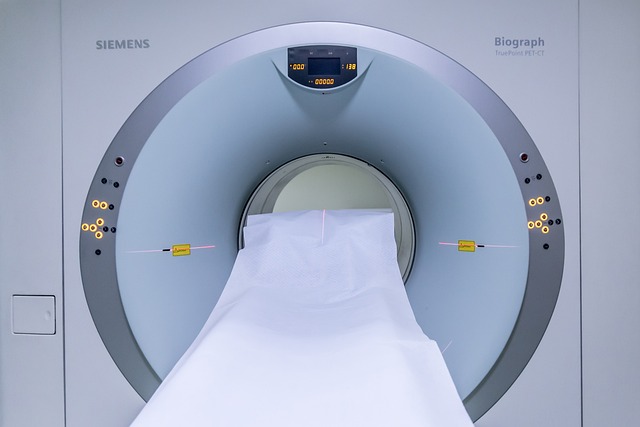
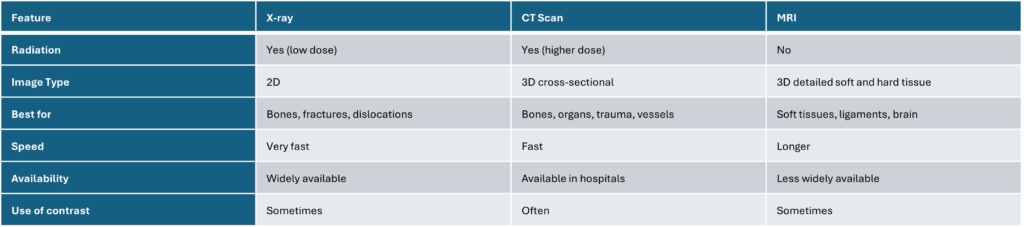
| Portable imaging (MRI/CT) | Quick, reliable upload of large imaging files from mobile units to specialists |
| Smart medication dispensers | Connected dispensers enable secure tracking of medicine adherence and timely remote adjustments |
| IoMT devices | Massive connectivity allows for device swarms in hospitals, managing logistics & safety |
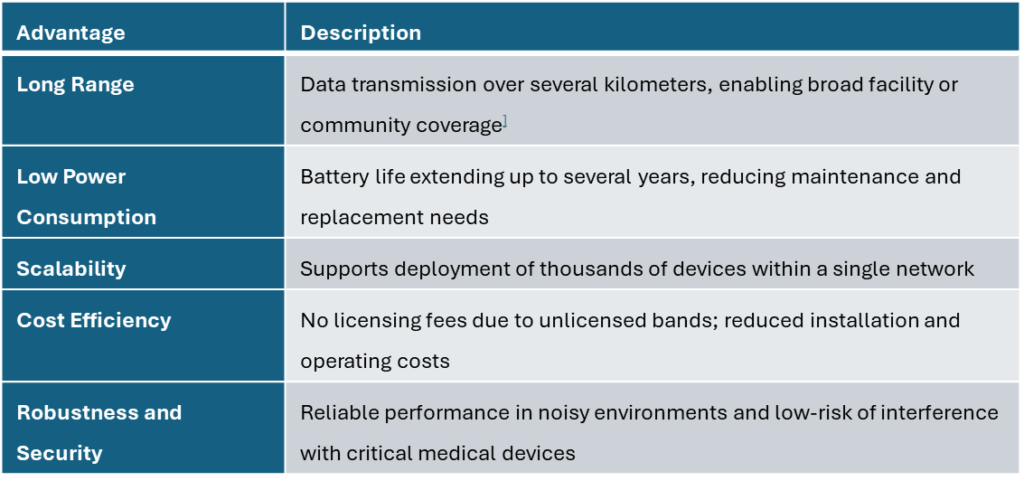
Key Advantages and Challenges
Advantages
Latency as low as 1 millisecond, vital for life-critical remote procedures and instantaneous alerts.
Bandwidth is exponentially increased, supporting simultaneous connections of thousands of devices per hospital or clinic.
Enhanced reliability ensures essential health services are prioritized, particularly in emergencies.
Expanding access to quality care for remote, rural, or underserved populations, reducing geographic barriers.
Challenges
Data security and privacy: The vast increase in connected devices and data transfer broadens the potential attack surface and requires robust security frameworks.
Integration: Updating legacy systems and ensuring interoperability with new 5G-enabled devices may require significant investment and planning.
Regulatory compliance: Adherence to evolving standards is crucial, as devices and networks must comply with healthcare regulations worldwide.
Conclusion
5G technology is revolutionizing medical networks, digital health, and medical devices by enabling faster, more reliable, and interconnected healthcare. Its benefits are seen across telemedicine, remote monitoring, connected medical devices, and AI-powered analytics, leading towards a future of patient-centric and accessible care—especially for those in remote locations. Successful adoption will depend on robust cybersecurity, seamless integration, and regulatory compliance.
Sources
https://pmc.ncbi.nlm.nih.gov/articles/PMC8764898
https://sequenex.com/the-impact-of-5g-on-connected-devices
https://pmc.ncbi.nlm.nih.gov/articles/PMC10007389
https://www.medicaldevice-network.com/sponsored/how-5g-is-changing-the-medical-device-landscape
https://www.sciencedirect.com/science/article/pii/S2949866X23000011
https://nybsys.com/5g-in-healthcare
https://www.uk-cpi.com/5g-in-healthcare
https://galendata.com/how-5g-is-impacting-connected-medical-technology