Environmental factors like air pollution, climate change, and water contamination significantly influence human health, contributing to a quarter of the global disease burden. These effects span respiratory, cardiovascular, and infectious diseases, with vulnerable groups including children, the elderly, and those with preexisting conditions, here some insight into related topics:
- Environmental influence on human health
- How does climate change specifically impact respiratory diseases
- What policies can mitigate environmental factors affecting health
- How can individuals protect themselves from environmental health threats
- What are the most effective strategies to reduce air pollution health risks
- What new research is emerging on environmental toxins and health
- HealthTech Advances on environmental health 2025
Environmental influence on human health
Air Pollution Impacts
Air pollution triggers respiratory issues such as asthma attacks, COPD worsening, and lung cancer, alongside cardiovascular problems like heart attacks and strokes. It also links to premature deaths, preterm births, diabetes, and cognitive impairments, with fine particles penetrating deep into lungs.
Climate Change Effects
Rising temperatures and shifting weather patterns increase heat-related illnesses, vector-borne diseases, and mental health issues like anxiety from displacement. They exacerbate mortality, respiratory and cardiovascular outcomes, and infectious disease transmission.
Water Contamination Risks
Contaminated water causes gastrointestinal illnesses, nausea, diarrhea, and long-term risks like cancer from chronic exposure to metals or chemicals. Vulnerable populations face heightened kidney, liver, and neurological damage.
How does climate change specifically impact respiratory diseases
Climate change exacerbates respiratory diseases primarily through prolonged pollen seasons, increased aeroallergens, higher ground-level ozone and particulate matter levels, and more frequent wildfires and heatwaves. These factors directly aggravate conditions like asthma, COPD, and rhinosinusitis while heightening infection risks.
Asthma Exacerbations
Warmer temperatures and elevated CO2 boost pollen production and allergenicity, extending seasons and triggering asthma attacks, especially during thunderstorms that rupture pollen into respirable particles. Wildfire smoke PM2.5 sharply increases emergency visits and hospitalizations for asthma.
COPD Worsening
Heatwaves and humidity fluctuations provoke COPD flares by worsening air pollution and dehydration, with studies showing higher mortality in temperature ranges of 3.8–29.9°C. Wildfire exposures link to mixed but often elevated ED visits and hospitalizations, particularly from fine particulates.
Additional Mechanisms
Mould proliferation from floods and droughts fuels respiratory infections and allergies, while ozone from heat intensifies inflammation. Vulnerable groups, including those with preexisting cardiopulmonary issues and low-income populations, face amplified risks.
What policies can mitigate environmental factors affecting health
Policies targeting emission reductions, urban planning, and cross-sectoral collaboration effectively mitigate environmental factors like air pollution, climate change, and water contamination that harm health. These measures lower disease burdens from respiratory issues, infections, and heat-related illnesses by addressing root causes.
Air Quality Regulations
Enforce strict limits on pollutants such as PM2.5, NO2, and ozone through WHO-aligned guidelines, industrial emission controls, and low-emission zones to cut respiratory and cardiovascular risks. Promote clean transport via incentives for electric vehicles and public transit expansion.
Climate Adaptation Frameworks
Adopt structured approaches like CDC’s BRACE framework to anticipate impacts, project disease burdens, and prioritize interventions such as urban greening and heat-resilient infrastructure. Policies protecting forests and habitats buffer against disease spread and extreme weather.
Water and Waste Management
Implement sanitation regulations, Clean Water Act-style standards, and waste controls to reduce waterborne diseases and chemical exposures, with health impact assessments ensuring targeted enforcement. Integrate health sectors with energy, agriculture, and transport for co-benefits like reduced pollution.
How can individuals protect themselves from environmental health threats
Individuals can shield themselves from environmental health threats like air pollution, extreme weather, and contaminated water through daily habits, home adjustments, and awareness tools. These actions reduce exposure to pollutants that exacerbate respiratory diseases, infections, and heat stress.
Monitor and Plan Exposure
Check real-time air quality via apps or websites to avoid outdoor activities on high-pollution days, staying indoors with windows closed during peaks. Track weather alerts for heatwaves or storms to limit time outside, especially for vulnerable groups like children or those with asthma.
Enhance Indoor Air
Use HEPA-filter air purifiers and exhaust fans to trap fine particles and allergens indoors, avoiding smoking, candles, or wood fires. Ventilate with filtered systems rather than opening windows in polluted areas, and shower after outdoor exposure to remove contaminants.
Protective Gear and Lifestyle
Wear N95 masks outdoors during poor air quality or wildfire smoke, and choose exercise locations away from traffic. Opt for filtered water, reduce personal emissions by walking or using public transport, and maintain a diet rich in antioxidants to bolster respiratory defenses.
What are the most effective strategies to reduce air pollution health risks
Effective strategies to reduce air pollution health risks combine policy-driven emission cuts, urban planning, and personal protective measures, with WHO guidelines emphasizing reductions in key pollutants like PM2.5 and ozone for maximum benefits. These approaches lower respiratory exacerbations, cardiovascular events, and premature deaths, particularly for vulnerable groups.
Adopt WHO Air Quality Guidelines with strict limits on PM, NO2, SO2, O3, and CO to drive emission reductions from industry, transport, and energy. Implement low-emission zones, promote public transport and cycling infrastructure, and enforce tobacco regulations alongside occupational exposure controls.
Expand green spaces with low-allergy trees, create car-free zones and superblocks, and separate pollution sources from residences and schools to cut exposure. Address energy poverty through cleaner heating to reduce indoor pollution from solid fuels.
Stay indoors during high pollution alerts, use HEPA air filters to lower indoor PM2.5, and limit outdoor exertion near traffic or on poor air days. Wear certified facemasks outdoors when needed, track air quality apps, and exercise away from roads.
What new research is emerging on environmental toxins and health
merging research highlights how environmental toxins like PFAS, microplastics, nano-plastics, and wildfire smoke increasingly threaten health through bioaccumulation, microbiome disruption, and novel toxicity pathways.
PFAS and Microbiome Interactions
Studies from 2024-2025 show gut bacteria can bioaccumulate PFAS, potentially mitigating internal exposure, with companies like Cam-biotics developing microbial interventions based on University of Cambridge research. PFAS links to immune, reproductive, and metabolic disorders, with ongoing EPA assessments of health risks.
Microplastics and Nano plastics
New toxicology employs omics technologies, organ-on-a-chip models, and high-throughput screening to reveal size-dependent hepatotoxicity of nano-silica and microplastics’ ties to cancer, heart issues, and inflammation in human cells and animals. Preschoolers face broad chemical exposures, including these particles.
2025 research connects Canadian wildfire smoke to worsened childhood asthma symptoms, while toxins accumulate in organic animal tissues, entering food chains. One Health approaches emphasize source control for contaminants like plastic-derived toxins.
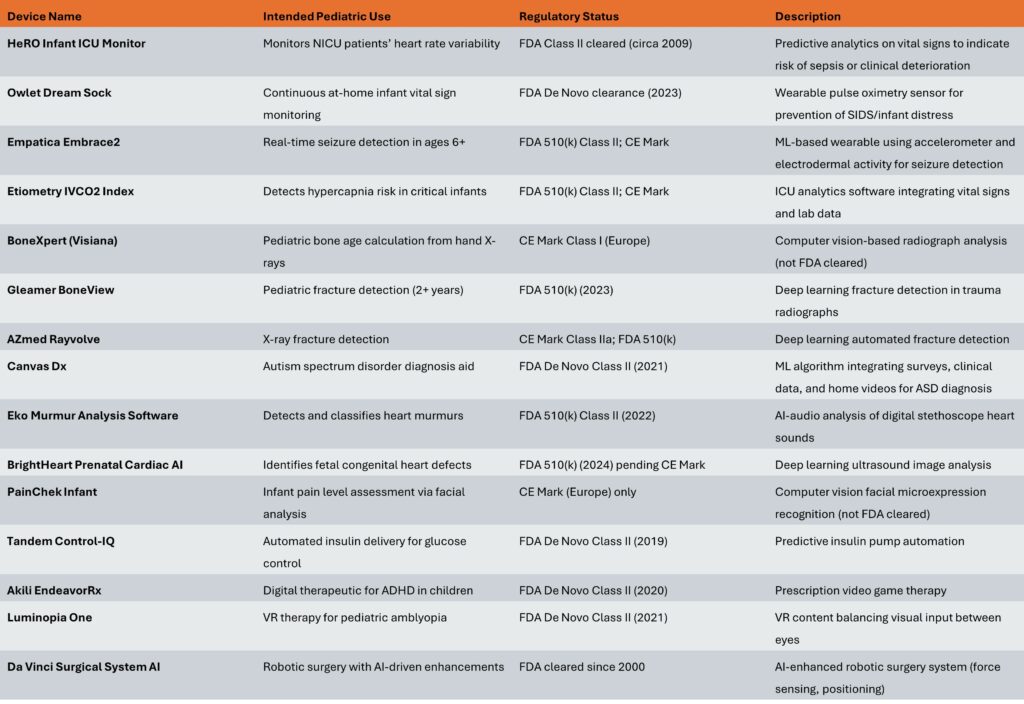
HealthTech Advances on environmental health 2025
HealthTech in 2025 is increasingly focused on “planetary health” – linking human health outcomes directly to climate, pollution, and ecosystem stability. The most active areas are AI, IoT, new materials, and sustainable care delivery models.
Environmental health tech in 2025 clusters around five themes: AI for prediction, pervasive sensing, sustainable materials and energy, low‑carbon clinical care, and citizen engagement. These technologies aim to both reduce health systems’ own footprint and manage climate‑ and pollution‑driven disease burdens.
Key technologies and use cases
AI and automation are used for exposure‑risk prediction (air, water, heat), compliance automation, and optimizing industrial and hospital processes to cut emissions and accidents.[5][1]
IoT and remote monitoring networks track air quality, water safety, workplace hazards, and building performance in real time, enabling earlier intervention for asthma, cardiovascular risk, and occupational disease.
Digital twins of hospitals, factories, or cities simulate environmental scenarios (heatwaves, pollution episodes, ventilation changes) to stress‑test resilience and optimize energy use, flows, and infection control before implementing changes physically.
Planetary health and infrastructure
Planetary‑health reports highlight 10 emerging solutions such as AI‑enhanced Earth observation, precision fermentation, green ammonia, methane capture, modular geothermal, regenerative desalination, and soil‑health tech, all framed as health‑relevant climate tools.
Green materials like CO₂‑mineralizing “green concrete” can lock captured CO₂ into infrastructure and reduce cement emissions, with regulatory uptake reported in Europe and North America.
Health systems and sustainability
Healthcare organizations increasingly integrate environmental, health, and safety into unified EHS strategies tied to carbon‑neutrality and zero‑waste targets.
Sustainable care trends include decarbonizing supply chains and facilities, expanding virtual care to avoid travel, and aligning consumer health offerings with lower‑impact behaviors (plant‑based nutrition, eco‑conscious fitness, etc.).
Engagement, data, and policy angles
Agencies and health systems deploy portals, apps, and social channels to share localized environmental‑risk data and co‑design community mitigation actions, improving environmental literacy and response.
Investment and strategy reports for 2025 note that environmental and planetary‑health angles are now a mainstream value driver in HealthTech funding, influencing due‑diligence, regulation, and ESG metrics.
If you share whether you care more about clinical pathways (e.g., heat‑stroke, asthma) or infrastructure/supply‑chain decarbonization, the focus can be narrowed to specific solution types and example vendors.
Have a look as well here
Link Collection
https://www.who.int/health-topics/environmental-health
https://www.lung.org/research/sota/health-risks
https://pubmed.ncbi.nlm.nih.gov/39517336
https://pmc.ncbi.nlm.nih.gov/articles/PMC8191619
https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health
https://coepht.colorado.gov/public-drinking-water-and-your-health
https://www.poison.org/articles/contaminated-water https://pmc.ncbi.nlm.nih.gov/articles/PMC11545045/
https://pmc.ncbi.nlm.nih.gov/articles/PMC9487563
https://pmc.ncbi.nlm.nih.gov/articles/PMC7386356
https://pmc.ncbi.nlm.nih.gov/articles/PMC11790401
https://pmc.ncbi.nlm.nih.gov/articles/PMC6743728
https://www.sciencedirect.com/science/article/abs/pii/S0013935123012525
https://jogh.org/2024/jogh-14-03032
https://pmc.ncbi.nlm.nih.gov/articles/PMC12476873
https://pubmed.ncbi.nlm.nih.gov/27300144
https://pubmed.ncbi.nlm.nih.gov/37352955
https://www.who.int/news-room/fact-sheets/detail/climate-change-heat-and-health
https://www.epa.gov/arc-x/public-health-resiliency-strategies
https://dialnet.unirioja.es/descarga/articulo/10070520.pdf
https://pmc.ncbi.nlm.nih.gov/articles/PMC12350827
https://www.who.int/health-topics/environmental-health
https://pmc.ncbi.nlm.nih.gov/articles/PMC12052406
https://pmc.ncbi.nlm.nih.gov/articles/PMC8494774
https://www.eea.europa.eu/en/newsroom/news/tackling-pollution-and-energy-poverty
https://www.sciencedirect.com/science/article/abs/pii/S2213260023003296
https://en.wikipedia.org/wiki/Environmental_health_policy
https://www.eea.europa.eu/en/topics/in-depth/environmental-health-impacts
https://www.sciencedirect.com/science/article/abs/pii/S0301479723024349
https://odphp.health.gov/healthypeople/objectives-and-data/browse-objectives/environmental-health
https://airly.org/en/5-tips-to-protect-yourself-from-unhealthy-air
https://pmc.ncbi.nlm.nih.gov/articles/PMC7270362
https://pubmed.ncbi.nlm.nih.gov/34936825
https://pmc.ncbi.nlm.nih.gov/articles/PMC4311076
https://www.epa.gov/p2/what-you-can-do-about-pollution-prevention
https://ehs.ucr.edu/coronavirus/protection
https://www.greencitytimes.com/10-ways-to-promote-environmental-awareness
https://www.who.int/health-topics/environmental-health
https://fsc.org/en/blog/ways-to-help-the-environment
https://www.un.org/en/actnow/ten-actions https://www.eea.europa.eu/en/topics/in-depth/environmental-health-impacts
https://pmc.ncbi.nlm.nih.gov/articles/PMC7270362
https://pmc.ncbi.nlm.nih.gov/articles/PMC12052406
https://www.eea.europa.eu/en/newsroom/news/tackling-pollution-and-energy-poverty
https://pmc.ncbi.nlm.nih.gov/articles/PMC8494774
https://www.sciencedirect.com/science/article/abs/pii/S2213260023003296
https://pubmed.ncbi.nlm.nih.gov/34936825
https://pmc.ncbi.nlm.nih.gov/articles/PMC4311076
https://www.who.int/europe/publications/i/item/WHO-EURO-2024-9115-48887-72806 https://pmc.ncbi.nlm.nih.gov/articles/PMC3018496/
https://www.epa.gov/pfas/our-current-understanding-human-health-and-environmental-risks-pfas
https://pmc.ncbi.nlm.nih.gov/articles/PMC12390250
https://www.sciencedirect.com/science/article/pii/S266667582400050X
https://phys.org/news/2025-11-persistent-environmental-toxins-accumulate-animal.html https://www.sciencedirect.com/science/article/pii/S2949750725000331
https://www.weforum.org/publications/10-emerging-technology-solutions-for-planetary-health
https://www.weforum.org/stories/2025/01/health-technology-global-healthcare
https://www.nrep.org/blog/future-ehs-trends-and-skills-2025
https://www.medparkhospital.com/ja-JP/lifestyles/10-health-trends-of-2025
https://seedblink.com/blog/2025-05-30-europes-healthtech-investment-landscape-in-2025-a-deep-dive
https://www.jpmorgan.com/insights/markets-and-economy/outlook/2025-healthtech-trends https://time.com/7318034/worlds-top-healthtech-companies-2025-methodology/